Fluorescent LFA vs Traditional Testing — What Healthcare Systems Should Know
OncoFirm Diagnostics | https://oncofirmdiagnostics.com
1. Executive Summary
Healthcare systems worldwide are under pressure to improve diagnostic speed, accuracy, and accessibility while controlling costs. As a result, there is growing interest in fluorescent lateral flow assay (FLFA) technologies—an evolution of traditional lateral flow assays (LFA). This whitepaper compares FLFA with conventional diagnostics, outlines their differences, and highlights the clinical and operational advantages that FLFA offers, especially in cancer diagnostics.
2. The Problem with Traditional Diagnostics
Traditional diagnostic testing—such as ELISA, immunohistochemistry (IHC), and imaging—has several limitations:
- Infrastructure-dependent: Requires centralized labs, specialized equipment, and trained technicians
- Slow turnaround: Days or weeks to receive results
- High cost per test: From reagents to labor, expenses quickly add up
- Limited access: Inaccessible for many low-resource or remote healthcare settings
In the face of these limitations, healthcare systems risk late diagnoses, delayed treatment, and higher costs of care.
3. Rise of Lateral Flow Assays (LFA)
LFA technology revolutionized rapid testing by enabling point-of-care diagnostics—quick, low-cost, and easy-to-use formats such as pregnancy tests or COVID-19 antigen kits.
Pros:
✅ Portable and equipment-free
✅ Fast results (5–30 min)
✅ Low cost and scalable
✅ Ideal for decentralized healthcare
Cons:
❌ Generally lower sensitivity
❌ Limited multiplexing (single-analyte detection)
❌ No digital quantification or low signal visibility
This is where fluorescent LFA (FLFA) steps in.
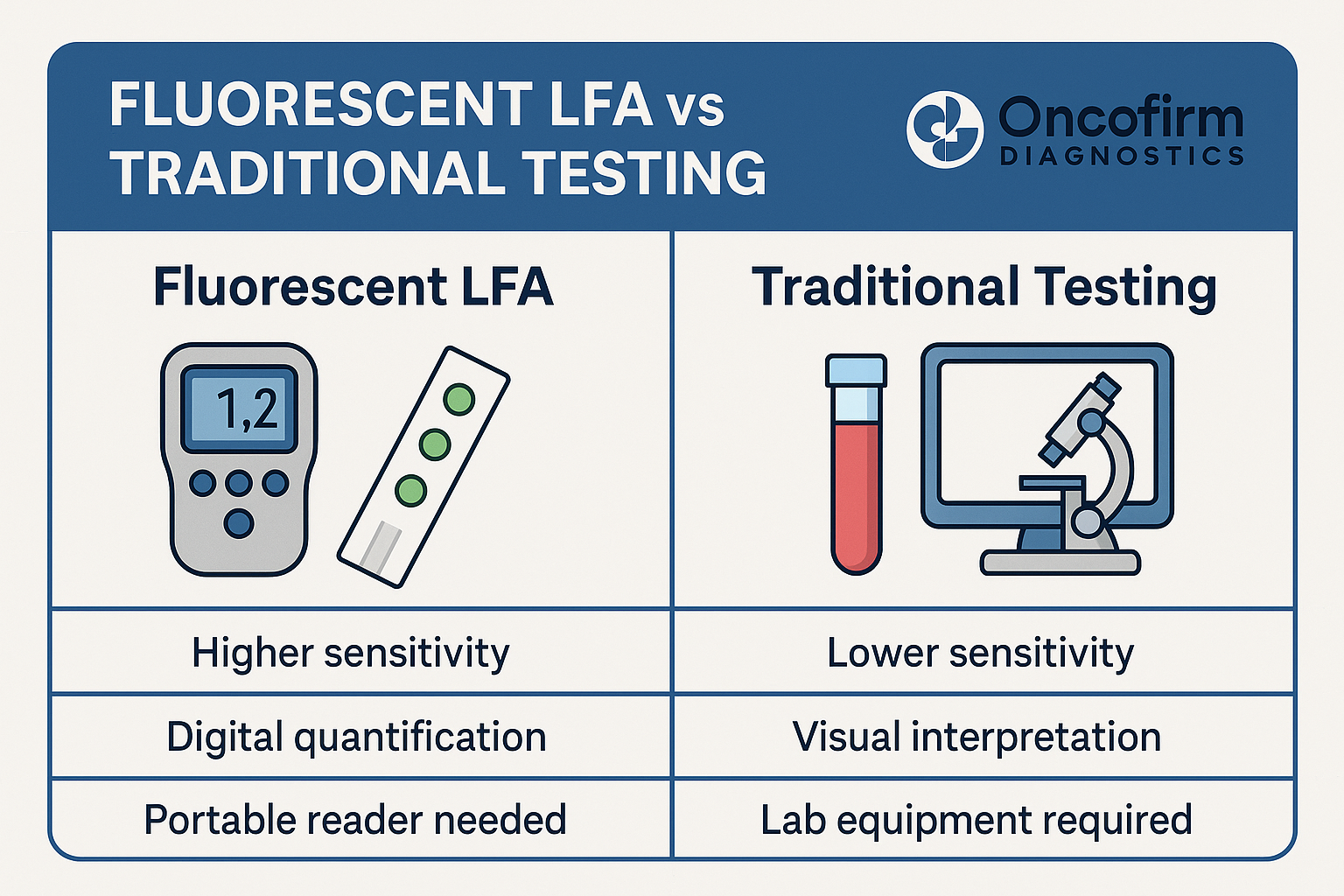
4. What Is Fluorescent LFA (FLFA)?
Fluorescent lateral flow assay (FLFA) is an enhanced version of LFA that uses fluorescent particles or dyes instead of colorimetric (visible) indicators. This allows for higher sensitivity, multiplexed detection, and digital quantification.
Key Features of FLFA:
| Feature | Traditional LFA | Fluorescent LFA (FLFA) |
|---|---|---|
| Detection method | Colorimetric (e.g. gold) | Fluorescent nanoparticles |
| Sensitivity | Moderate | High (up to 10x improvement) |
| Quantification | Visual (subjective) | Digital (objective readout) |
| Multiplexing | Limited | Up to 4–5 targets per strip |
| Reader device needed? | No | Yes (portable or smartphone-based) |
| Cost per test | Low | Moderate |
| Use case | Single-target quick tests | Multi-target diagnostics |
5. Why FLFA Is Critical for Cancer Diagnostics
Cancer detection demands extreme accuracy, specificity, and early detection—making FLFA particularly well-suited.
Benefits of FLFA in Oncology:
- Detects low-abundance biomarkers that traditional LFA would miss
- Enables multiplexed cancer screening in one strip (e.g., breast + colorectal + lung)
- Supports quantitative monitoring of biomarker trends over time
- Improves diagnostic performance while remaining portable and fast
6. OncoFirm’s FLFA Innovation
OncoFirm Diagnostics is pioneering next-generation fluorescent LFA cancer screening tests using newly identified tumor antigens linked to disease progression.
OncoFirm Technology Highlights:
- Proprietary cancer-specific antigens (e.g., Thomsen–Friedenreich antigen)
- Multiplex panel for major solid tumors: colorectal, breast, lung, prostate, pancreatic, and liver
- Digital reader integration for data capture and EMR integration
- Sub-15-minute results without the need for laboratory infrastructure
OncoFirm’s platform is engineered to bridge the diagnostic gap in both developed and resource-limited settings.
7. Use Cases for Healthcare Systems
A. Primary Care Clinics
Enable family doctors to screen high-risk patients in-office without referring to labs.
B. Remote & Rural Health Programs
Deploy mobile screening units with FLFA tools for early detection in underserved populations.
C. Oncology Pathways
Speed up the diagnosis-to-treatment pipeline by reducing wait times from weeks to minutes.
D. Global Health NGOs
Roll out early cancer diagnostics in LMICs where traditional labs are scarce or non-existent.
8. Implementation Considerations
| Topic | Traditional Testing | FLFA Considerations |
|---|---|---|
| Infrastructure | Central labs, lab techs | Handheld reader device, training |
| Cost per Test | High | Moderate, scalable |
| Accuracy | High (but slow) | Comparable or superior |
| Throughput | Limited by lab workflow | Point-of-care deployment |
| Patient Experience | Invasive, delayed results | Quick, non-invasive |
9. Conclusion
Healthcare systems face a choice: continue relying on centralized, costly diagnostics—or evolve toward affordable, fast, decentralized testing with fluorescent LFA technology.
OncoFirm Diagnostics offers a powerful solution that merges speed, precision, and accessibility—setting a new benchmark for early cancer detection. For hospitals, governments, NGOs, and health systems, FLFA presents a game-changing tool in the battle against cancer.
10. Learn More
Visit https://oncofirmdiagnostics.com or contact us to access our investor deck, clinical validation roadmap, or distribution opportunities.
📧 Contact: info@oncofirmdiagnostics.com